Veterinary Burnout: Causes, Prevention & Tech
- CoVet

- Jul 30, 2025
- 8 min read
Updated: Jan 8
Burnout in veterinary medicine isn’t just common, it’s becoming the norm. A 2022 Merck Animal Health study found that over 50% of veterinarians experience high levels of burnout, with younger DVMs and support staff feeling the pressure most.*
Between long hours, emotional strain, and rising client demands, many veterinary professionals are reaching a breaking point. It’s taking a toll not just on mental health, but also on team morale, patient care, and long-term career satisfaction.
You might recognize it in yourself or your team: exhaustion before the day even starts, frustration during routine consults, or medical records piling up after hours.
The good news? Burnout isn’t inevitable. By understanding what causes it—and putting the right tools and strategies in place—you can protect your wellbeing and create a more sustainable way to work.
Understanding the root causes of veterinary burnout
Veterinary burnout builds over time, often from a mix of emotional, logistical, and systemic stressors. Here are some of the most common contributors:
Long working hours: Between back-to-back appointments, emergency cases, and paperwork after hours, most clinic teams work far beyond their scheduled shifts.
Emotional exhaustion from difficult cases: Euthanasia decisions, chronic illnesses, and seeing pets in pain—especially when paired with emotional owners—can leave even seasoned vets and techs emotionally depleted.
Compassion fatigue: When you’re constantly giving empathy without enough recovery time, it wears you down. Many veterinary professionals start to feel numb or detached as a protective response.
Financial stress: High student loan debt, relatively low pay compared to workload, and the pressure to meet revenue goals can leave staff feeling undervalued and stretched thin.
Client expectations and confrontations: Dealing with emotional, impatient, or demanding pet owners adds another layer of pressure—especially when costs, treatment plans, or tough news are involved.
Staff shortages: Whether due to hiring challenges or turnover, thin staffing means fewer hands on deck and more responsibilities for each team member.
Lack of work-life balance: When clinical responsibilities bleed into personal time, recovery becomes impossible. Many DVMs report staying late just to finish veterinary record keeping, cutting into evenings, weekends, and rest.
Burnout symptoms and warning signs to look out for
Veterinary burnout doesn’t always look like someone breaking down mid-shift. More often, it creeps in quietly—until you or your teammates are running on empty. These are some of the most common signs to watch for:
Physical and mental exhaustion
Feeling drained before your shift even begins
Trouble sleeping or waking up unrested
Frequent headaches, tension, or GI issues
Emotional changes
Loss of empathy or becoming emotionally numb toward patients and clients
Irritability, mood swings, or emotional outbursts
Increased cynicism or detachment from the job
Behavioral shifts
Declining job performance or missing clinical details
Avoiding certain tasks, patients, or conversations
Withdrawing from coworkers or team collaboration
Reduced career satisfaction
Feeling like your work doesn’t matter—or questioning if you should stay in the field
Frustration with routine cases that once felt meaningful
A sense of hopelessness about things improving
These symptoms can show up in anyone on the team—not just the DVMs. Techs, assistants, receptionists, and managers are just as vulnerable. Recognizing these red flags early is the first step toward creating a healthier clinic environment.
Practical, research-backed burnout prevention strategies
There’s no one-size-fits-all fix for burnout, but that doesn’t mean it’s untouchable. The best strategies are the ones that address both personal wellbeing and clinic-wide systems. Here’s how individuals and practices can take action:
For individuals (e.g., DVMs, RVTs, Techs, Assistants)
Prioritize self-care—consistently, not just occasionally
You can’t pour from an empty cup. That means setting boundaries around rest, meals, hydration, and screen time—even on busy days. Skipping breaks might feel productive in the moment, but it adds up fast. Even 10 minutes to eat, breathe, or step outside between appointments can recharge your focus and mood.
Try mindfulness-based practices
Mindfulness is a proven way to calm your nervous system and reset between emotionally intense cases. Whether it’s a short meditation in your car, a breathing app between appointments, or jotting down three things that went well after a shift—it creates mental space so stress doesn’t build unchecked.
Access support through Employee Assistance Programs (EAPs)
If your clinic or employer offers an EAP, make it part of your toolkit. These programs often include confidential access to licensed counselors, financial wellness resources, and mental health support—all designed to help you cope before you hit a breaking point. And if your clinic doesn’t offer one? It might be time to advocate for it.
Set and communicate professional boundaries
Burnout accelerates when we feel like we have to say “yes” to everything. Whether it’s responding to client texts at 9 p.m., working through lunch, or taking on an extra shift, it’s okay—and healthy—to say no when needed. Setting boundaries also means being clear with your team about what you can reasonably take on.
Build emotional resilience through continuing education
Learning how to cope is just as important as learning clinical skills. Workshops on compassion fatigue, peer support groups, or even CE courses focused on mental health can give you the tools to manage the emotional load that comes with the job. It’s also a way to normalize these conversations in veterinary medicine—something the field sorely needs.
For practices (e.g., HMs, PMs)
Implement flexible scheduling when possible
You may not be able to reduce caseloads, but you can give your team more control over how they work. Rotating on-call duties, adjusting shift lengths, or even piloting 4-day workweeks can help staff recover between high-intensity days. Flexibility doesn’t mean chaos—it means creating options that help prevent fatigue.
Encourage delegation and cross-training
When the whole team knows how to support each other, no one person carries the full weight. Teaching assistants to prep patients, techs to handle follow-ups, or reception to triage basic questions means DVMs and PMs can stay focused on their highest-value work. Delegation isn’t passing the buck—it’s working smarter as a unit.
Create an open feedback loop
Burnout festers in silence. That’s why structured, regular check-ins—whether anonymous surveys or team huddles—are essential. But it’s not just about gathering input. Show the team you’re listening by taking action, reporting back on what’s changed, and making continuous improvement part of your culture.
Invest in team communication
So many stressors come from miscommunication—missed instructions, unclear expectations, or tasks slipping through the cracks. Use tools or systems that make it easy to log updates, assign follow-ups, and share patient details in real time. Even something as simple as a shared digital note can reduce hallway confusion and repeated conversations.
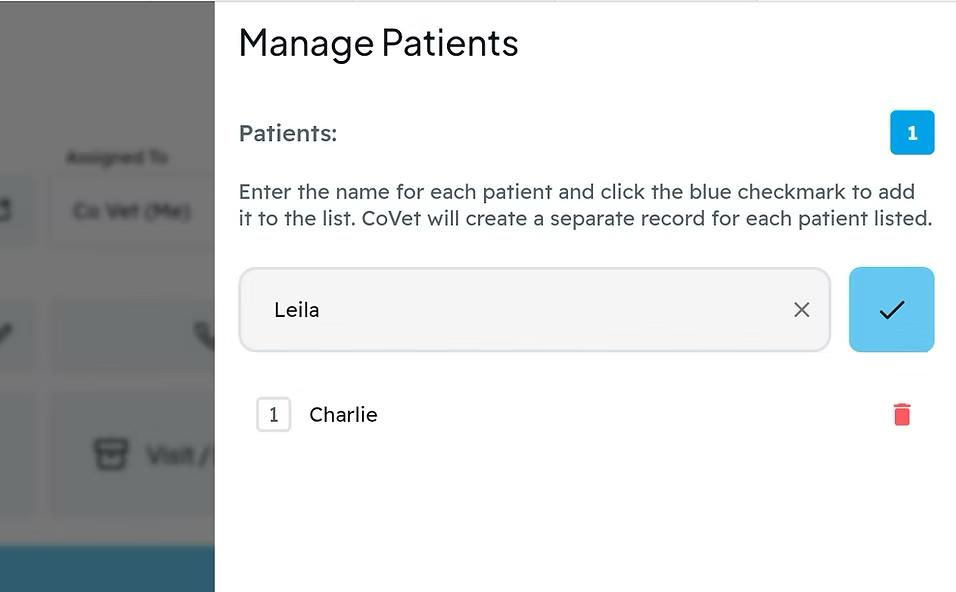
Solutions like CoVet, which allow teams to tag tasks or leave notes tied directly to patient records and multi-pet records, can help ensure everyone stays aligned—without relying on memory or sticky notes.
Foster a supportive clinic culture
This one’s big. Create a workplace where vulnerability isn’t punished, mistakes are learning opportunities, and mental health is taken seriously. Celebrate wins—no matter how small—and make “How are you doing?” a regular part of the workday. A clinic that feels psychologically safe is one where people stay longer and thrive.
Related article: Thinking about an exit? This guide breaks down how to sell a veterinary practice: what increases value, how buyers evaluate financials and operations, and what to tighten up before you go to market.
How AI scribes help reduce veterinary burnout
You can’t remove every stressor from veterinary medicine, but you can take one of the biggest ones off your plate: documentation. Understanding the difference between dictation vs transcription methods can help to reduce after-hours documentation.
AI scribes and veterinary dictation software are changing how clinics manage records by helping teams capture complete, structured notes in real time—without the after-hours load.
Here’s how they work—and why they matter:
Reduce time spent on documentation
Instead of typing SOAP notes, also known as medical notes, between appointments or late into the evening, AI scribes like CoVet allow you to speak naturally during or after an exam. The system listens, captures the key details, and turns them into formatted medical records—automatically. For many clinics, this means reclaiming hours of time every week and eliminating the dreaded post-shift documentation pile.

Lower cognitive load and free up mental space
When you’re juggling multiple cases, clients, and tasks, it’s easy to forget small but important details. CoVet helps reduce that mental strain by acting as a real-time second brain—logging SOAP notes, tracking flagged symptoms, and making it easier to stay focused on the patient in front of you. The result? Fewer mistakes, smoother handoffs, and more mental clarity.
Improve work-life balance and job satisfaction
Burnout thrives when work follows you home. By handling recordkeeping during the day—without interrupting your workflow—AI scribes make it easier to leave on time, stay present during personal hours, and reduce the emotional spillover from the job.
Fit into real veterinary workflows
CoVet was built specifically for clinic teams, not adapted from human healthcare or generic transcription tools. It works with your existing practice management system (PMS), supports real-time collaboration, and lets you tag team members for follow-ups or vitals. Whether you’re a solo DVM managing everything yourself or part of a multi-location hospital, the tool adapts to how you already work.
AI scribes don’t replace your clinical skills—they support them. Think of them as an invisible team member: one who never forgets a detail, never needs a reminder, and helps the whole clinic stay in sync.
Check out our guide of vet clinic software tools to streamline your operations.
Combat burnout with the right tools and support
Burnout in veterinary medicine is real, but it’s not unfixable. Recognizing the signs early, putting better habits in place, and creating a supportive clinic culture are all key steps toward protecting your team’s wellbeing and improving day-to-day life.
But individual strategies only go so far without the right systems to back them up. That’s where tools like AI scribes and copilots come in—removing repetitive tasks, reducing after-hours work, and keeping your team focused on care instead of catching up on records.
Advances in AI in veterinary medicine are making this possible for clinics of all sizes.
You don’t have to overhaul your entire clinic to make a difference. Start with one or two changes. Try a flexible schedule pilot. Run a burnout check-in during your next team meeting. Or explore how CoVet could support your staff behind the scenes, every day.

Frequently asked questions about veterinarian burnout
What are some veterinary burnout causes?
Veterinary burnout stems from long hours, emotional exhaustion from tough cases, compassion fatigue, financial pressures, demanding clients, staff shortages, and poor work-life balance.
The emotional toll of euthanasia and chronic illness cases, combined with heavy administrative tasks like veterinary record keeping, creates stress. These factors make burnout common across veterinary teams, affecting mental health and job satisfaction.
What is compassion fatigue in veterinary medicine?
Compassion fatigue occurs when continuous empathy and emotional support for sick or suffering animals deplete a vet’s emotional reserves. It can cause numbness, detachment, or irritability, impacting care quality and personal wellbeing. Recognizing compassion fatigue early is crucial to preventing deeper veterinary burnout.
What are some veterinarian burnout symptoms?
Common symptoms include physical and mental exhaustion, irritability, emotional numbness, reduced empathy, poor job performance, withdrawal from colleagues, and declining job satisfaction. According to common veterinary burnout statistics, these signs often go unnoticed until they severely impact wellbeing and clinic culture.




